
In 1841, US President William Henry Harrison died only 32 days into his only term in office. The killer was a common culprit in Harrison’s day, one destined to end the life of Stephen A. Douglas of the famous Lincoln/Douglas debates, William “Willy” Lincoln (right), the 11-year-old son of President Abraham & First Lady Mary Todd Lincoln, and Martha Bulloch Roosevelt, mother of President Theodore Roosevelt.
Historians blame Typhoid fever for the plague that killed the great statesman Pericles and a third the population of Athens, in 430BC. “America’s first epidemic”, Typhoid killed some 85 percent of the settlers in the English colony at Jamestown between 1607 and 1624. Among native American populations, Typhoid fever was a “virgin soil disease” leading to widespread outbreaks among indigenous populations.
In 1880, German pathologist Karl Joseph Eberth first described the bacillus involved while, throughout the 19th century, Typhoid could be counted on to kill more combatants than any given war in which they had come to fight.
There’s no polite way to say it. Typhoid is spread by fecal contamination between humans. Today, simple acts like flushing a toilet and washing one’s hands are parts of daily routine. In an age before modern plumbing and sewage, we’re talking about a plague sufficient to make the bogey man himself, quake with terror.
Even now, sciencemag.org reports some ten to thirty million cases per year and somewhere around 200,000 deaths worldwide each year. Today, scientists across the African continent and Asia contend with the multi-drug resistant strain H58, but now we’re ahead of the story. In a century beginning with the Napoleonic wars and ending with the gilded age, the “germ theory” of disease we now know so well rose only gradually to the fore, eclipsing the “miasma” theory so familiar to contemporaries of the Black Death.
Like the Chinese Coronavirus of another century, Typhoid symptoms range from excruciating death to nothing whatsoever. Mary Mallon was one of the latter. Born in 1869 in the north of Ireland, Mary was almost certainly infected in utero even as her mother was so tainted, at the time of birth.
Mary emigrated to the United States at age fifteen and lived for a time with an aunt and uncle. She worked as a maid at first but it didn’t take long to realize…Mary Mallon could cook. Soon she was hiring on with wealthy families as a personal chef.
In 1906, New York banker Charles Henry Warren arranged a treat for his family. A summer rental seemed just the thing. Warren rented the summer home of George Thompson and his wife in Oyster Bay, Long Island. Naturally, Warren went looking for a cook. Mary Mallon accepted the job.
That August, one of the Warren daughters fell ill with Typhoid fever. Mrs. Warren was soon to follow and then two maids. In total, six of eleven people in the household came down with the disease. Fearing they wouldn’t be able to rent the place, Thompson hired investigators to find the cause.

That first group found nothing and Thompson hired George Soper, a civil engineer known even then as, the “epidemic fighter”. It was Soper who first hypothesized that Mary herself, might be the cause. At this point, Mallon had left the family three weeks earlier. Soper examined Mallon’s employment history from 1900 to the present, and there it was. There were seven jobs during that time in which 22 people became ill, with Typhoid. One little girl died of the disease shortly after Mary came to work for the family.
The civil engineer turned “private eye“ went looking for Mary herself. He found her in March 1907, working for the family of one Walter Bowen.
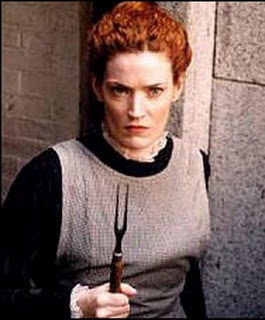
Soper explained who he was and requested samples of Mary’s blood, urine and feces. Mallon responded in a fashion to be expected of a cornered wildcat. With a shriek and a carving fork she came at him, putting the man to flight.
Once again Soper tracked her down and showed up where she lived. This time, he brought help in the person of Dr. Bert Raymond Hoobler. And now there were two of them, fleeing for their lives.
Dr. Sara Josephine Baker was dispatched from the New York city health department but by now, Mallon wasn’t hearing a word of it. Next came Soper with five police officers, and an ambulance. Let the epidemic fighter describe what happened next.
“Now thoroughly convinced of her own persecution, “Mary was on the lookout and peered out, a long kitchen fork in her hand like a rapier. As she lunged at me with the fork, I stepped back, recoiled on the policeman and so confused matters that, by the time we got through the door, Mary had disappeared. ‘Disappear’ is too matter-of-fact a word; she had completely vanished”
George Soper
There followed a five-hour cat & mouse before they found her, hiding in a closet. It took several of them to wrestle Mary to the ground. Soper himself sat on her all the way to the hospital. He said it was like being in a cage with an angry lion.
Mary was taken to Willard Parker hospital where stool samples demonstrated the presence of Typhoid. Under questioning she admitted to “almost never” washing her hands, a practice not uncommon at that time. There followed a period of incarceration between 1907 and 1910 on North brother island on the East River, near the Bronx.
The press had a field day with the story. “Typhoid Mary” they called her.
“I never had typhoid in my life, and have always been healthy. Why should I be banished like a leper and compelled to live in solitary confinement with only a dog for a companion?”
Mary Mallon

During that time, 120 of 163 samples tested positive. Mary herself couldn’t understand why she was being treated this way. She had broken no laws. She’d been taken by force and against her will. She had a nervous breakdown. Her own samples smuggled out with the help of a friend, tested negative. She sued for her freedom. And lost. The courts didn’t want anything to do with it. Soper would visit from time to time and sometimes explained the importance of handwashing. She wasn’t buying any of it. Why…Would… They…DO THIS TO ME!? It was all she could think of.
In 1910, Mary was released to the mainland with an agreement t0 “take such hygienic precautions as will protect those with whom she comes in contact, from infection.” She promised not to accept work as a cook. Soon she was working as a laundress, earning $20 a month, without a home of her own, and teetering on the brink of destitution. She used to make $50 a month, as a cook.
It wasn’t long before she broke her word. Now it was “Marie Breshof” or “Mrs. Brown,” cooking for a restaurant on Broadway, or a hotel in Southampton. There was an inn in Huntington. A sanatorium in New Jersey. Her cooking gigs were always short-term and always followed by Typhoid outbreaks.
Then came the job at Sloan Hospital for Women. 20 people fell ill with Typhoid. Two died. Even the other other servants came to call the new cook, “Typhoid Mary”.
This time when they came for her, she didn’t resist. On March 27, 1915, Mary Mallon was returned to quarantine on North Brother Island. She had a stroke there in 1932 and spent the last six years of her life, partly paralyzed. She contracted pneumonia and died there on Armistice Day, November 11, 1938. Nine people attended her funeral.

Over her lifetime, Typhoid Mary is believed to have sickened no fewer than fifty, three of whom died. Some put her death toll as high as fifty. In a nation of laws the civil liberties side of her story stands to this day as an historic, unmitigated, disaster. Mary Mallon spent her last years alone in this small house on North Brother Island in the East River, near the Bronx

The history of Mary Mallon, declared “unclean” like a leper, may give us some moral lessons on how to protect the ill and how we can be protected from illness…By the time she died New York health officials had identified more than 400 other healthy carriers of Salmonella typhi, but no one else was forcibly confined or victimized as an “unwanted ill”.
The Annals of Gastroenterology, 2013















 Ordinary flu strains prey most heavily on children, elderly, and those with compromised immune systems. Not this one. This flu would kick off a positive feedback loop between small proteins called cytokines, and white blood cells. This “cytokine storm” resulted in a death rate for 15 to 34-year-olds twenty times higher in 1918, than in previous years.
Ordinary flu strains prey most heavily on children, elderly, and those with compromised immune systems. Not this one. This flu would kick off a positive feedback loop between small proteins called cytokines, and white blood cells. This “cytokine storm” resulted in a death rate for 15 to 34-year-olds twenty times higher in 1918, than in previous years.










 In the mid-19th century, birthing centers were set up all over Europe, for the care of poor and underprivileged mothers and their illegitimate infants. Care was provided free of charge, in exchange for which young mothers agreed to become training subjects for doctors and midwives.
In the mid-19th century, birthing centers were set up all over Europe, for the care of poor and underprivileged mothers and their illegitimate infants. Care was provided free of charge, in exchange for which young mothers agreed to become training subjects for doctors and midwives.





































You must be logged in to post a comment.